Traveler’s Diarrhea (Infant/Toddler)
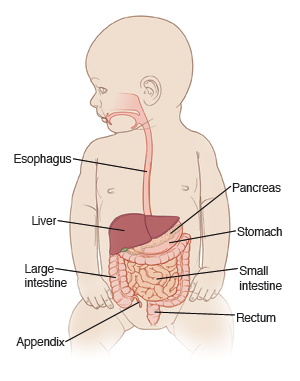
Traveler’s diarrhea is an infection in the intestinal tract. It's usually caused by bacteria called E. coli. These bacteria are often found in water supplies in less developed countries. The local people of those countries are immune to E. coli and don’t get sick. Tourists who drink water or eat foods that were washed or prepared with this water may become very ill.
The illness begins 1 to 3 days after exposure. It can last up to 5 days, or sometimes longer. Symptoms include fever, vomiting, stomach cramps, and watery diarrhea. There may be blood or mucus in the stool. Mild cases will get better without treatment. Antibiotics are used for more severe cases.
The main danger from this illness is dehydration. This is the loss of too much water and minerals from the body. When this happens, body fluids must be replaced. This can be done with oral rehydration solution (ORS). Oral rehydration solution is available at pharmacies and most grocery stores. In more severe cases, fluids may need to be given by IV (intravenously, with a catheter into a vein).
Home care
Follow all directions given by your child’s health care provider.
If giving medicine to your child:
-
Don’t give over-the-counter diarrhea medicines unless your child’s provider tells you to.
-
If antibiotics were prescribed, make sure your child takes them every day until they are finished. Don’t stop giving them if your child feels better. Antibiotics must be taken as a full course.
-
You can use acetaminophen or ibuprofen to control pain and fever. Or you can use other medicine as prescribed. Don't give aspirin to children or teens unless your child’s doctor says it is safe. Aspirin can put your child at risk for Reye syndrome, a rare but serious condition.
-
Sometimes your child's provider will prescribe medicine to stop the vomiting. Give it only as directed. If the vomiting continues with taking the medicine, contact your child's provider.
To prevent the spread of illness:
-
Remember that washing with soap and water is the best way to prevent the spread of infection.
-
Wash your hands before and after caring for your sick child.
-
Clean the toilet after each use.
-
Dispose of soiled diapers in a sealed container.
-
Keep your child out of daycare until your child's provider says it's OK.
-
Wash your hands before and after preparing food.
-
Wash your hands after using cutting boards, countertops, and knives that have been in contact with raw foods.
-
Keep uncooked meats away from cooked and ready-to-eat foods.
-
Keep in mind that people with diarrhea or vomiting should not prepare food for others.
Giving liquids and feeding
The main goal while treating vomiting or diarrhea is to prevent dehydration. This is done by giving small amounts of liquids often. Liquids are the most important thing. Don’t be in a rush to give food to your child.
If your baby is breastfed:
-
Keep breastfeeding. Feed your child more often than usual.
-
If diarrhea is severe, give oral rehydration solution between feedings.
-
As diarrhea decreases, stop giving oral rehydration solution and resume your normal breastfeeding schedule.
If your baby is bottle-fed:
-
Give small amounts of fluid at a time, especially if your child is vomiting. Give 1 to 2 ounces of fluid every 30 minutes. This may improve symptoms.
-
Give full-strength formula or milk. If diarrhea is severe, give oral rehydration solution between feedings.
-
Don’t give apple juice, soda, or other sweetened drinks. Drinks with sugar can make diarrhea worse.
-
If your child is doing well after 24 hours, resume a regular diet and feeding schedule.
-
If your child starts doing worse with food, go back to clear liquids.
If your child is on solid food:
-
Keep in mind that liquids are more important than food right now. Don’t be in a rush to give food.
-
Don’t force your child to eat, especially if they are having stomach pain, cramping, vomiting, or diarrhea.
-
Don’t feed your child large amounts at a time, even if they are hungry. This can make your child feel worse. You can give your child more food over time if they can tolerate it.
-
Give small amounts at a time, especially if your child is having stomach cramps or vomiting.
-
If diarrhea is severe, give ORS between feedings.
-
If your child is doing well after 24 hours, try giving age-appropriate solid foods. These can include cereal, oatmeal, bread, noodles, mashed carrots, mashed bananas, mashed potatoes, applesauce, dry toast, crackers, soups with rice noodles, yogurt, lean meats, fruits, and cooked vegetables. Avoid high-fat foods since they are harder to digest.
-
If your child starts doing worse with food, go back to clear liquids.
-
You can resume your child's normal diet over time as they feel better. If the diarrhea or cramping gets worse again, go back to a simple diet or clear liquids.
Follow-up care
Follow up with your child’s health care provider, as advised. If a stool sample was taken or cultures were done, call the provider for the results as directed.
Call 911
Call 911 if your child has:
When to call your child's doctor
Contact your child’s health care provider right away if your child has:
-
Belly pain that gets worse.
-
Constant lower right belly pain.
-
Swollen belly.
-
Repeated vomiting after the first 2 hours on liquids.
-
Occasional vomiting for more than 24 hours.
-
Continued severe diarrhea for more than 24 hours.
-
A small amount of blood in stool or vomit.
-
A refusal to drink or feed.
-
Dark urine or no urine for 8 hours, no tears when crying, sunken eyes, or dry mouth.
-
Fussiness or crying that cannot be soothed.
-
A new rash.
-
More than 8 diarrhea stools within 8 hours.
-
Diarrhea lasts more than 1 week on antibiotics.
-
A fever (see Fever and children, below).
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the health care provider what type to use instead. When you talk with any provider about your child’s fever, tell them which type you used.
Below is when to call the provider if your child has a fever. Your child’s provider may give you different numbers. Follow their instructions.
When to call a doctor about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider